
Imagine this: In one wing of a hospital, a premature baby is placed on a ventilator. Under the same roof, a baby the same age is being aborted. Former respiratory therapist AJ Hurley saw this dichotomy firsthand, and it made him realize the urgency of ending abortion.
Now as the Director of Activism at Live Action, one of the nation’s leading pro-life advocacy groups, AJ has dedicated his career to saving the lives of the unborn. He’ll tell us his story as he went from working as a medical professional to a pro-life activist, the story of Baby Olivia, and how you can join him and Live Action in saving lives and ending abortion.
WATCH TODAY on Facebook, Twitter, or YouTube!
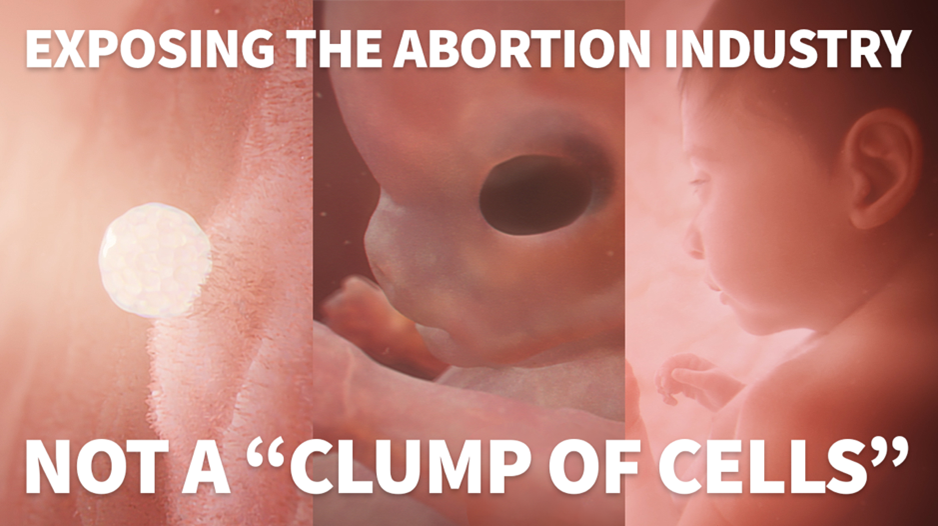
(Or by clicking the image below)
1:00pm PT / 2:00pm MT / 3:00pm CT / 4:00pm ET
At Family Policy Alliance, our vision is a nation where God is honored, religious freedom flourishes, families thrive, and life is cherished. To stay up to date on the fight to protect families and learn how to take action, follow us on social media!
See you in the comments section! 

Emma Rarden
Communications Specialist- Producer
P.S. Have you checked out our NEW podcast? We pick the brains of newsmakers and experts to break down what’s happening now on the issues YOU care about. With new episodes weekly, you’ll be up to date on all things that affect your family. Listen on Spotify, Apple Podcasts, or Google Podcasts.

